Download Value-based Care Contracting Dictionary PDF Here
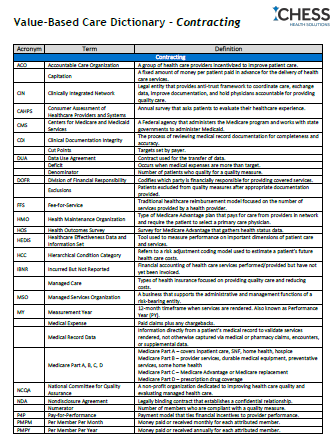
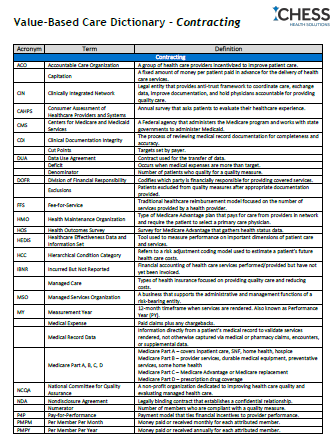
| Acronym | Term | Definition |
|---|---|---|
| ACO | Accountable Care Organization | A group of health care providers incentivized to improve patient care. |
| Capitation | A fixed amount of money per patient paid in advance for the delivery of health care services. | |
| CIN | Clinically Integrated Network | Legal entity that provides anti-trust framework to coordinate care, exchange data, improve documentation, and hold physicians accountable for providing quality care. |
| CAHPS | Consumer Assessment of Healthcare Providers and Systems | Annual survey that asks patients to evaluate their healthcare experience. |
| Cut Points | Targets set by payer. | |
| DUA | Data Use Agreement | Contract used for the transfer of data. |
| Deficit | Occurs when medical expenses are more than target. | |
| Denominator | Number of patients who quality for a quality measure. | |
| DOFR | Division of Financial Responsibility | Codifies which party is financially responsible for providing covered services. |
| Exclusions | Patients excluded from quality measures after appropriate documentation provided. | |
| FFS | Fee-for-Service | Traditional healthcare reimbursement model focused on the number of services provided by a health provider. |
| HMO | Health Maintenance Organization | Type of Medicare Advantage plan that pays for care from providers in network and require the patient to select a primary care physician. |
| HOS | Health Outcomes Survey | Survey for Medicare Advantage that gathers health status data. |
| HEDIS | Healthcare Effectiveness Data and Information Set | Tool used to measure performance on important dimensions of patient care and services. |
| IBNR | Incurred But Not Reported | Financial accounting of health care services performed/provided but have not yet been invoiced. |
| Managed Care | Types of health insurance focused on providing quality care and reducing costs. | |
| MSO | Managed Services Organization | A business that supports the administrative and management functions of a risk-bearing entity. |
| Measurement Year | 12-month timeframe when services are rendered. Also known as Performance Year (PY). | |
| Medical Expense | Paid claims plus any chargebacks. | |
| Medical Record Data | Information directly from a patient’s medical record to validate services rendered, not otherwise captured via medical or pharmacy claims, encounters, or supplemental data. | |
| Medicare Part A, B, C, D | Medicare Part A – covers inpatient care, SNF, home health, hospice Medicare Part B – provider services, durable medical equipment, preventative services, some home health Medicare Part C – Medicare Advantage or Medicare replacement Medicare Part D – prescription drug coverage | |
| NDA | Nondisclosure Agreement | Legally binding contract that establishes a confidential relationship. |
| Numerator | Number of members who are compliant with a quality measure. | |
| P4P | Pay-for-Performance | Payment model that ties financial incentives to provider performance. |
| PMPM | Per Member Per Month | Money paid or received monthly for each attributed member. |
| PMPY | Per Member Per Year | Money paid or received annually for each attributed member. |
| Percent of Premium | The proportion of direct medical expenses incurred for care to total premiums paid to the plan. Also known as Medical Loss Ratio (MLR). | |
| PPO | Preferred Provider Organization | Type of Medicare Advantage plan where patients have the option to see specialists and any provider in or out of network. |
| PDC | Proportion of Days Covered | According to Pharmacy Quality Alliance (PQA), the percent of days in the measurement period covered by prescription claims for the applicable medication(s). |
| PEX | Provider Engagement Exchange | |
| Reporting Year | Timeframe when final data is reported for the measurement year, usually the year following the performance year. | |
| Risk | Payment model that requires the provider to refund the payer for any losses incurred if financial benchmarks/medical loss ratio are exceeded. | |
| Risk Bearing Entity | An organization that assumes financial responsibility for cost of care. | |
| Shared Savings | Payment model that compares total spending to a target. | |
| Stop Loss | A product that provides protection against catastrophic or unpredictable losses. | |
| Surplus | Occurs when medical expenses are less than target. |