
Hierarchical Condition Category (HCC) coding is a tool for ensuring accurate risk adjustment and appropriate reimbursement. For healthcare providers, effectively managing HCC recapture is not just about compliance – it’s about delivering better patient outcomes and sustaining financial health.
What is HCC Recapture?
HCC recapture involves revalidating and documenting chronic conditions for patients annually. Because conditions not documented in a given year may not be reflected in risk adjustment calculations, the recapture process is essential for maintaining an accurate representation of patient complexity. Without proper HCC coding, organizations risk underpayments and missed opportunities to allocate resources effectively for high-need patients.
Why HCC Recapture Matters
- Accurate Risk Adjustment: Risk scores drive reimbursement in many value-based care models. Capturing all relevant HCCs ensures funding aligns with the true complexity of a patient population.
- Improved Patient Care: Regularly reviewing and recapturing conditions promotes proactive management of chronic diseases.
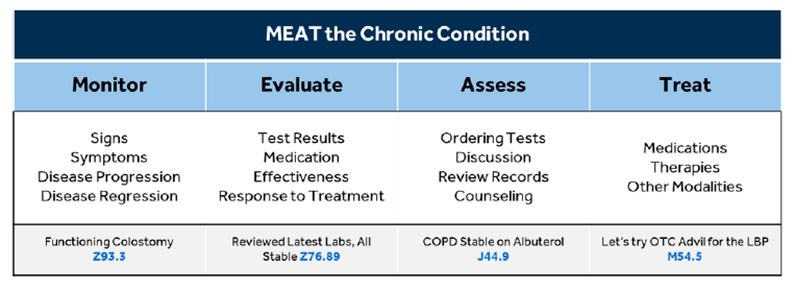
- Compliance and Audits: Proper documentation of current monitoring, evaluation, assessment, and/or treatment (MEAT) mitigates the risk of penalties associated with coding errors or underreporting.
Strategies for Successful HCC Recapture
- Annual Wellness Visits: Use AWVs to review and document chronic conditions comprehensively. These visits offer an opportunity to engage with patients while updating medical records.
- Leverage Technology: EHR tools and analytics can identify missed HCCs or patients due for recapture. Predictive algorithms can flag gaps in coding and documentation.
- Provider Education: Train providers on the importance of HCC documentation, including specificity in coding and the annual recapture process. Encourage accurate use of ICD-10 codes and emphasize how coding impacts reimbursement and care quality.
- Interdisciplinary Collaboration: Work closely with care managers, coders, and other team members to ensure coding accuracy. Sharing insights across departments helps identify missed opportunities and streamline workflows.
- Audits and Feedback: Conduct regular chart audits to monitor compliance and coding accuracy. Provide feedback to providers to address recurring gaps or errors.
- Documentation: Provide accurate and complete documentation for diagnoses, coding chronic conditions to the highest specificity.
Best Practices for Documentation
Each coded and billed diagnosis must have supporting documentation in the encounter note for the date of services.
Ensure documentation MEATs the criteria below:
Effective HCC recapture is a cornerstone of success in value-based care. By prioritizing accurate documentation, leveraging technology, and fostering collaboration among care teams, healthcare providers can ensure compliance, improve patient outcomes, and sustain financial stability.

