
Not all quality measures intended for the general adult population may be appropriate for people with limited life expectancy or advanced illness and frailty. The National Committee for Quality Assurance (NCQA) implemented exclusions across many Healthcare Effectiveness Data and Information Set (HEDIS) measures to redirect focus to those who will benefit the most from measured services.
The Exclusion Criteria is important if:
- You have patients with advanced illness
- Some screenings and services seem unnecessary for your complex patients
- You’re responsible for open care gaps for patients who refuse screenings or treatment because they are too sick
For individuals 65 years of age and older who have an advanced illness and frailty, the following measures can be impacted:
- Breast cancer screening
- Colorectal cancer screening
- Comprehensive diabetes care
- Controlling high blood pressure
- Kidney health evaluation
- Osteoporosis management in women with a fracture
- Statin therapy for patients with diabetes and heart disease
These exclusions help ensure quality measures and all associated quality improvement efforts focus on the population most likely to benefit from the specified services.
There are benefits of the advanced illness and frailty exclusions, including:
- Increased focus on care that is more appropriate for a patient’s health status
- Reduction of unnecessary screening and testing
- Improved management of patients and their treatment
- Reduced administrative efforts
For patients to be excluded from a quality measure, there must be documentation of an advanced illness AND frailty condition coded on a claim each calendar year.
HEDIS Exclusions
This information reflects HEDIS specifications but does not replace clinical judgment. A healthcare provider’s clinical judgment should always guide treatment decisions.
Codes for advanced illness identify patients who will be removed from the impacted measures’ eligible populations. Patients can only be excluded through appropriate and applicable documentation and coding on submitted claims.
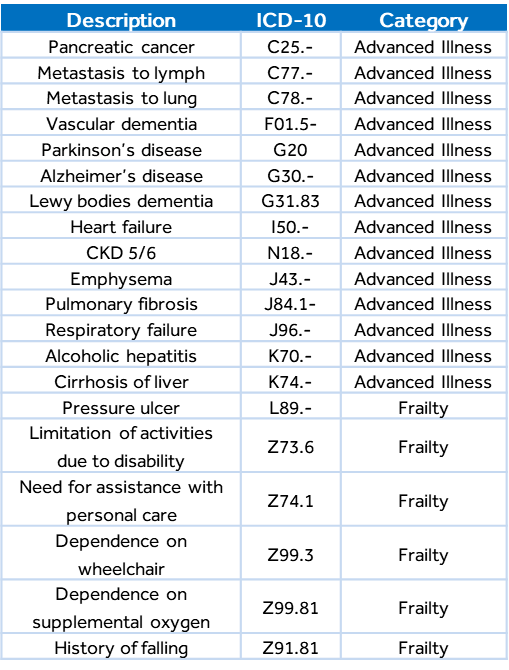
Below is a non-inclusive list of common diagnosis codes for each category.
RESOURCES: NCQA; ICD-10-CM Guidelines; Humana
About the Author


