
The Patient Protection and Affordable Care Act of 2010 marked the beginning of the Medicare Wellness Visits program for Medicare beneficiaries 65 years and older. These visits focus on the identification of health risk factors, including Social Determinants of Health (SDOH), and accompany the development of an individualized prevention plan for each patient. This plan may include Advance Care Plan discussion and updates as indicated.
Now in the 14th year, the MWV program continues to have low performance rates for most primary care practices. Providers may view them as unnecessary and a waste of the typical 15–20-minute time allotment for a visit. Let’s look at these visits with alternative perspectives: contribution to value-based care and ambulatory patient safety.
Would you consider a procedure, surgery, or disease-specific intervention if the provider overseeing the event had no plan for the process and goal outcome? For example, surgery without the time out, instrument check, sterile field maintained, and post-operative plan? Probably not, as that would be unsafe. The participants would not know the correct order of the procedure, the aftercare required for the care team or home caregiver, and as a result, you might incur harm.
Medicare Wellness Visits are the equivalent of the plan of care for a patient’s risk factors and the primary, secondary, and tertiary testing/interventions needed to keep that patient in the best health possible. Through the preventive plan, the patient may receive a wide range of preventive services, many of which have no co-pay for the patient. The Annual Wellness Visit (AWV) is also the only time a patient has no co-pays for Advance Care Planning (ACP) or the Social Determinants of Health (SDOH) risk assessment. Both require patient consent. In a value-conscious environment, ACP discussions and documentation align the patient’s goals/values with advancing disease and end-of-life wishes. The SDOH risk assessment identifies deficits in the patient’s social milieu that may interfere with diagnosis or treatment plans.
That prevention plan becomes the core of safer care for the patient. How so? Just as in acute care settings, safety incidents occur in ambulatory settings. The most common incidents are diagnostic errors (missed or delayed), prescribing and medication management errors, and administrative and communication issues. In a 2015 study, these incidents occurred 2-3 times per 100 primary care visits, and another estimated that 5% of U.S. adult outpatients may have experienced a diagnostic error annually.
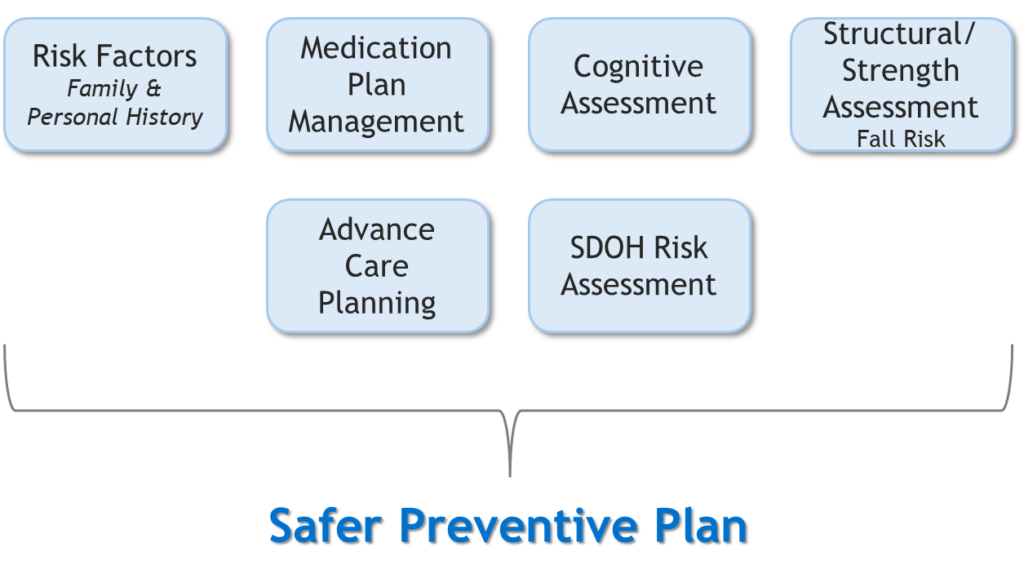
Unlike an illness-related visit, Medicare Wellness Visits focus on the total patient risks and associated prevention strategies. In the review of all medications, cognitive and structural strength, risk factors, and recommended preventive services in this visit, a safer plan for the next 5-10 years is developed and updated as the patient’s physical, social, or behavioral status changes. In developing that plan, utilization of expensive resources can be delayed or even prevented through ACPs in plan, inclusion of SDOH factors in the plan, and prescribing or de-prescribing of high-risk medications when indicated. The graphic below shows how this would work with an Annual Wellness Visit:
About the Author


