
The transition home after hospitalization is a high-risk period for Medicare beneficiaries. Poor transitions of care amount to over $25 billion in health expenditures for Medicare every year. Transitional Care Management (TCM) is a fee-for-service opportunity created by CMS to reduce hospital readmissions, ensuring patients receive the right care at the right time in the right place.
Importance of Transitional Care Management
Medicare beneficiaries often have complex health conditions and multiple comorbidities, making them particularly vulnerable during care transitions. Poorly managed transitions result in medication errors, unnecessary hospital readmissions, and adverse health complications. Effective Transitional Care Management is important for several reasons:
- Preventing Care Gaps: TCM addresses the critical hand-off period between inpatient and community settings, enabling continuity of care and preventing service gaps that can lead to negative health outcomes.
- Improving Patient Outcomes: Effective TCM reduces avoidable readmissions, improving health outcomes and satisfaction.
- Financial Benefits: The Medicare TCM program provides increased reimbursement for healthcare providers, supporting the sustainability of these essential services.
- Enhanced Patient Experience: Clear communication and continuity improve patient satisfaction and build trust.
TCM Components
When a patient is discharged from an approved inpatient setting, the following TCM components must be provided during the 30-day service period:
- Contact beneficiary/caregiver by phone, email, or face-to-face within two business days of discharge. The outreach must be more than scheduling an appointment.
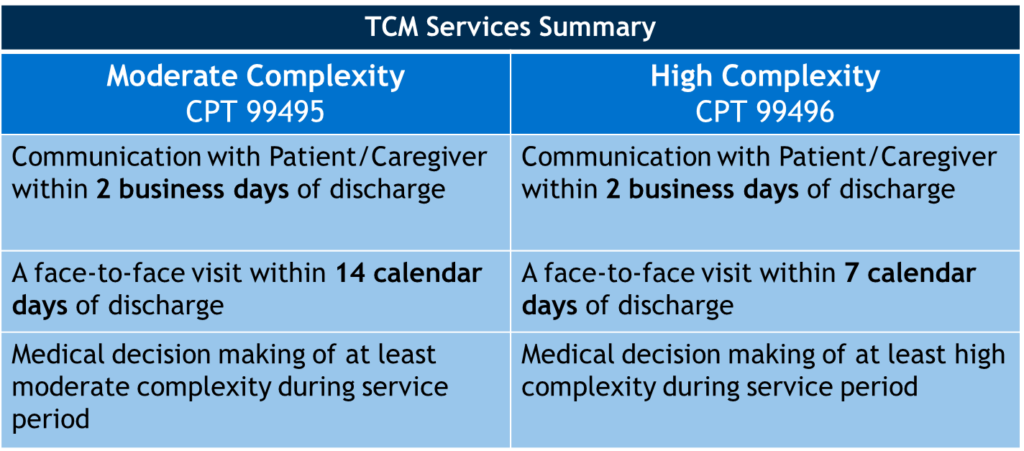
- Conduct a face-to-face visit within 7 or 14 days of discharge, depending on complexity of medical decision-making involved.
- Medication reconciliation and management completed on or before the face-to-face visit date.
- Review discharge information.
- Review the need for diagnostic tests/treatments and/or follow-up on pending diagnostic tests/treatments.
- Educate the patient, family, caregiver, and/or guardian.
- Establish referrals and arrange needed community resources (if applicable).
- Help schedule required providers and services follow-up (if necessary).
Billing TCM
CMS created two billing codes for Transitional Care Management (TCM) to improve coordination of care for Medicare patients across multiple care environments. These CPT codes, 99495 and 99496, recognize and compensate providers for the additional work required to support patients after discharge.
Technology’s Role in TCM
Technology improves care transitions by enhancing communication, coordination, and patient outcomes. Digital tools, like electronic health records (EHRs), enable seamless sharing of patient information across providers, reducing the likelihood of medical errors and promoting continuity of care. Technology platforms also facilitate the sharing of patient information across health systems, helping providers identify utilization outside of their organization. These utilization insights aid in the creation of leakage strategies to make sure all patients get support during transitions. Telehealth platforms expedite timely follow-up visits, allowing healthcare teams to identify potential complications early and intervene at the right time. Additionally, technology and artificial intelligence (AI) assist care teams in determining which patients to contact, how often, and when during the first 30 days after discharge to optimize outreach.
Transitional Care Management (TCM) services support healthy transitions after inpatient stays. These services decrease readmissions for high-risk patients by facilitating better communication among healthcare providers and ensuring no care gap post-facility discharge occurs. Transitions of Care support plays an integral role in utilization reduction and cost management, helping organizations meet value-based goals and remain financially sustainable.
About the Author


