Medicaid Services Model
CHESS has a deep understanding of the specific Medicaid challenges faced by North Carolinians. To address the unique needs of patients in our communities, we have developed a robust set of tools and resources that empower providers to deliver enhanced care for patients with complex needs.
Flexible Model & More Than Tech

Transformation Focused

Pop Health Driven by Real-Time Data

All-Patient
Solution
Medicaid Care Management
Navigate the Complexities of Managed Medicaid with an Experienced Partner.
We have the knowledge and tools necessary to help you better care for vulnerable populations in North Carolina.
• Over 12 Years of Care Management Experience
• Hands on Support – Care Managers Act as an Extension of Your Practice
• 29% Care Management Penetration Rate in 2023
• NCQA/Case Management Society of America Compliant Care Model – Meets AMH Tier 3 Requirements
• Proven Evidence-based Protocols and Workflows to Address SDoH and Enhance Patient Outcomes
• Comprehensive Care Management & Behavioral Health Assessments

CHESS offers robust care management services for North Carolina Managed Medicaid Standard Plans:
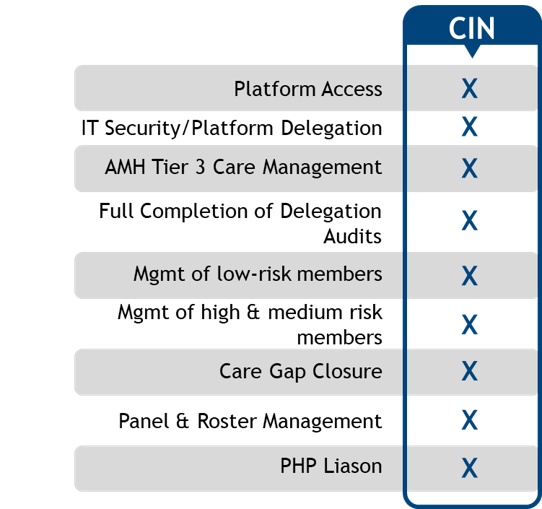
Medicaid CIN
Helping you better serve your Managed Medicaid population in North Carolina.
Our Clinically Integrated Network (CIN) is a group of healthcare providers that work together to deliver efficient and affordable care to patients.
The CHESS Medicaid CIN offers independent providers a pathway to enhanced care coordination, improved outcomes, and sustainable growth. By joining, providers gain access to the resources, tools, and incentives needed to thrive in an increasingly complex healthcare environment.

Committed to providing high-quality, patient-centered care, the CHESS Medicaid CIN brings together a diverse group of healthcare providers and organizations, seamlessly coordinating services to improve outcomes for Medicaid beneficiaries.
100% of Quality Payments Paid to Physicians
$1 PMPM Bonus for Meeting Citizenship Criteria

Compliant Population Health Platform
Ensure your data and analytics platform meets all AMH Tier 3 Medicaid requirements seamlessly. CHESS’ ready-to-use platform enables providers to handle the data ingestion, integration, reporting, and care management operations for Managed Medicaid Standard and Tailored Plans. Unified patient records, real-time data, and evidence-based protocols provide actionable insights at the point of care.
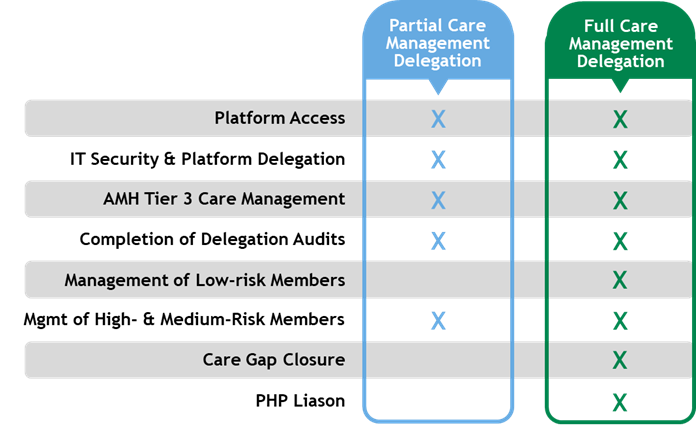
Right-Sized Care Management Delegation
Customized care management delegation for Standard Plans depending on your practice’s unique needs. Delegate the management of high- and medium-risk members or let CHESS handle the management of all members.
Clinically Integrated Network
The CHESS Medicaid CIN offers independent providers a pathway to enhanced care coordination, improved outcomes, and sustainable growth. By joining, providers gain access to the resources, tools, and hands on support needed to thrive in an increasingly complex healthcare environment.

